Clinical utility of TBS in bone health management
Trabecular Bone Score (TBS) provides clinicians with additional, valuable insights into bone quality and fracture risk, complementing information provided by Bone Mineral Density (BMD) and clinical risk factors or FRAX®.
What is TBS?
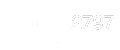
TBS is an innovative analytic method enriching fracture risk assessment. Utilizing a modified experimental variogram-based approach, the patented TBS algorithm interprets the complexity of the bone’s projected image, translating subtle grey-level pixel-by-pixel variations into an estimate of three-dimensional bone microarchitecture. This index exhibits a strong correlation with the intrinsic microarchitecture and mechanical competencies of bone, thus complementing the BMD T-score, which primarily evaluates bone quantity.
How BMD and TBS complement each other?
TBS provides additional information to BMD assessments. While BMD measures the quantity of mineral content in bone, TBS evaluates the bone microarchitecture. This distinction is important because two patients with the same bone density (same BMD values) can have a different underlying bone microarchitecture (different TBS scores). Therefore, they will not have the same fracture risk, due to variations in bone quality captured by TBS.
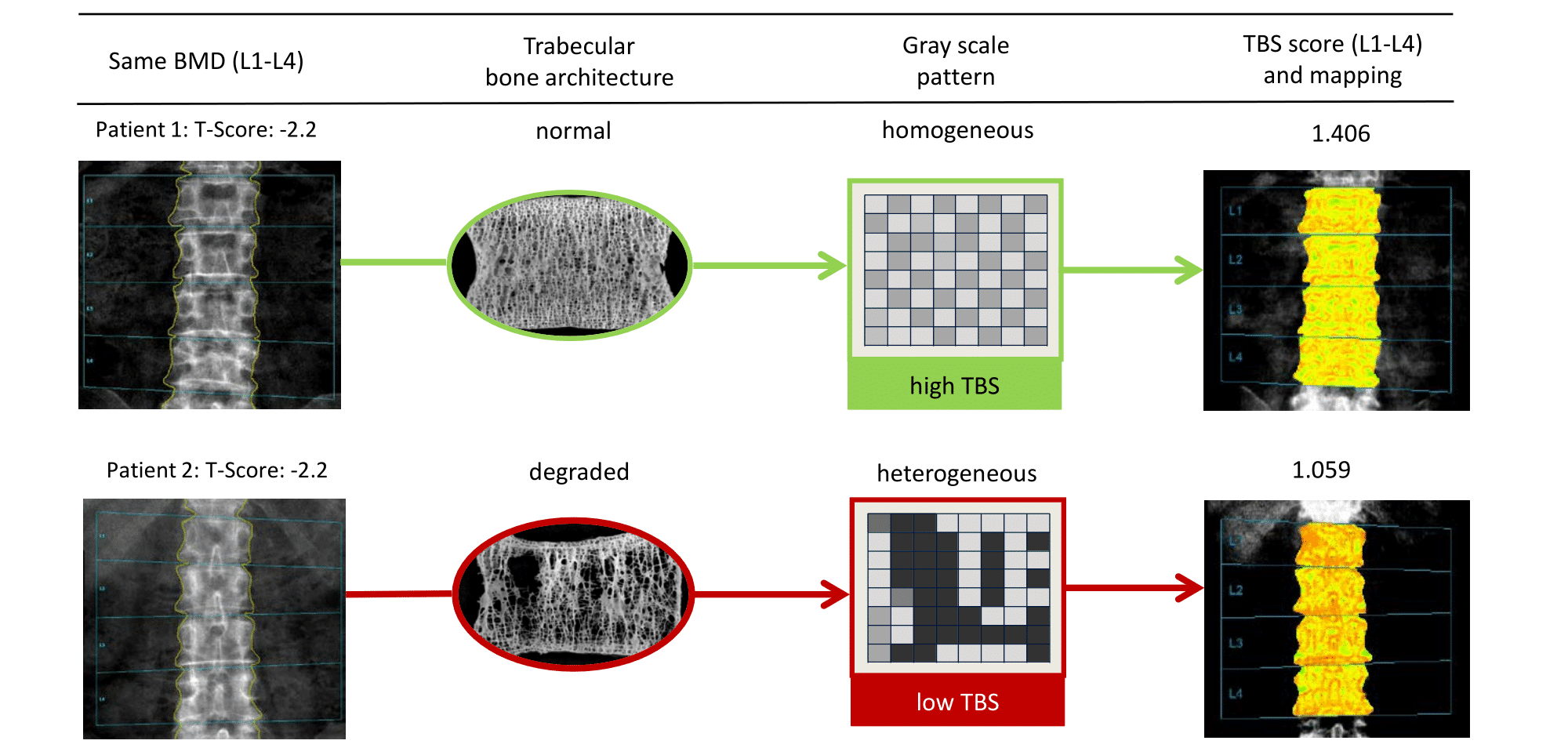
~30% of osteopenic patients are about the same risk of fracture as some of those who are osteoporotic1
The following table presents the level of fracture risk expressed as the number of major osteoporotic fractures per 1000 women/year. Risk stratification of TBS and BMD enhances the accuracy of fracture risk assessment, particularly in osteopenic patients and patients with secondary osteoporosis2. The table shows that about 30% of osteopenic patients are reclassified by adding TBS to BMD assessments.
Level of fracture risk based on classification of the World Health Organization
(based on a 5-year follow-up of the Manitoba study cohort of 30,000 women aged 50+ years)
Learn more about TBS
Download our white paper elucidating the scientific underpinnings, clinical utility, and the value of TBS in improving osteoporosis management and patient outcomes.
Clinical relevance
The efficacy of TBS in predicting fragility fracture is underpinned by over one decade of peer-reviewed research. The global research community has contributed to this evidence base with over 1,500 peer-reviewed publications, and the clinical utility of TBS is underscored by its widespread adoption—over 4.5 million TBS evaluations are performed annually across more than 90 countries.

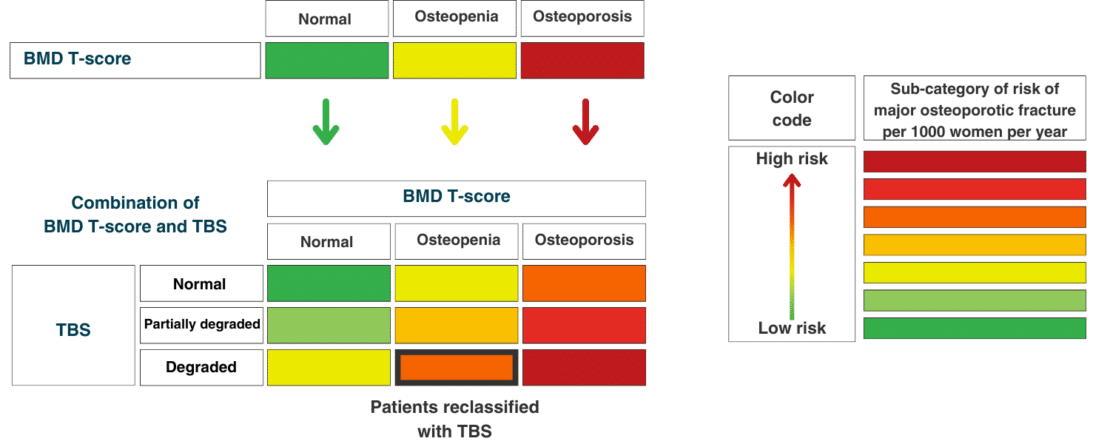
TBS Osteo is an AI-ready technology and state-of-the-art software powered by TBS iNsight to evaluate bone microarchitecture in patients during a DXA bone densitometry scan. It provides the missing link needed to identify more patients at risk of fracture.
1. Adapted from Hans D, Goertzen AL, Krieg MA, Leslie WD. Bone microarchitecture assessed by TBS predicts osteoporotic fractures independent of bone density: the Manitoba study. J Bone Miner Res. 2011;26(11):2762-2769. doi:10.1002/jbmr.499
2. Shevroja E, Reginster JY, Lamy O, et al. Update on the clinical use of trabecular bone score (TBS) in the management of osteoporosis: results of an expert group meeting organized by the European Society for Clinical and Economic Aspects of Osteoporosis, Osteoarthritis and Musculoskeletal Diseases (ESCEO), and the International Osteoporosis Foundation (IOF) under the auspices of WHO Collaborating Center for Epidemiology of Musculoskeletal Health and Aging. Osteoporosis Int. 2023;34:1501-1529.