Detecting osteoporosis: the importance of bone microarchitecture
Osteoporosis is a systemic skeletal disease characterized by diminished bone mass and the degradation of bone microarchitecture. These dual components — bone mass and bone microarchitecture — underpin the structural integrity necessary for bone resilience against fractures1.
Bone microarchitecture refers the structure of bone tissues at a microscopic level, including the connectivity of cancellous bone elements, the number of trabeculae and the size of trabecular spaces. Bone microarchitecture is a determinant aspect of bone strength and an essential element for the assessment of bone mechanical properties.
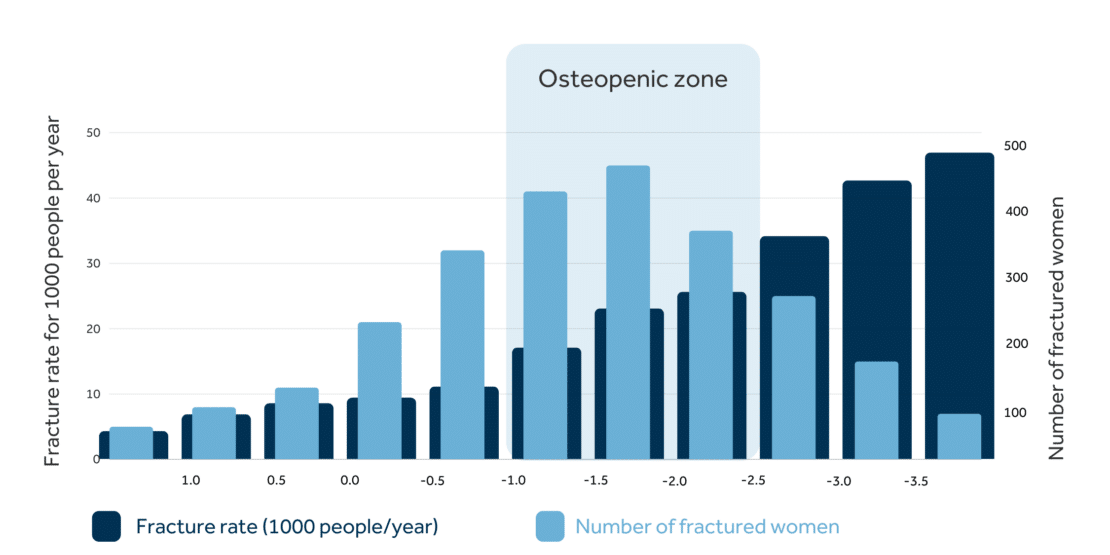
Traditional densitometric evaluations, centered around a bone mineral density (BMD) T-score of -2.5 or lower, capture the bone mass dimension of this risk, effectively discerning a subset of individuals predisposed to fragility fracture2. Yet, this approach does not fully address the spectrum of fracture risk, because most of these fractures occur in patients with T-scores outside the osteoporotic range2. A more comprehensive assessment framework is requisite — one that integrates bone microarchitecture, the second critical determinant of bone strength, to refine the identification of those at increased fracture risk.
Current challenges in osteoporosis
The global burden of fragility fractures is substantial, with around 9 million cases occurring annually, and at least one in three women and one in five men aged over the age of 50 years sustaining an osteoporotic fracture3. This equates to one major osteoporotic fracture every 3 seconds3. Such fractures, especially those of the hip and spine which are associated with significant pain and disability, bringing substantial burdens for patients, their families and healthcare systems. Of those patients who sustain a hip fracture, around one third will die within 12 months4. Current trends and demographic shifts predict a rise in the burden of osteoporosis, yet research demonstrates that a large proportion of fractures could be prevented with better risk identification5.
<In most cases, osteoporosis remains undiagnosed until a fracture occurs, highlighting the inadequacies of current risk assessment strategies. Although BMD is integral for determining bone mass, it does not address the microarchitectural quality of bone, which is a vital factor for bone strength. It is also noteworthy that over 70% of fragility fractures occur in women who are non-osteoporotic by BMD alone6 – which highlights a critical imitation of relying solely on BMD for risk stratification.
Evaluating bone microarchitecture: the role of Trabecular Bone Score
In addressing this clinical need, Trabecular Bone Score (TBS) is a pivotal advancement. TBS is an innovative analytic method that derives a grey-level textural index from dual-energy X-ray absorptiometry (DXA) scans, delivering a quantifiable assessment of bone microarchitecture. This index exhibits a strong correlation with the intrinsic microarchitecture and mechanical competencies of bone, thus complementing the BMD T-score and enriching fracture risk assessment7. Clinical application of TBS has demonstrated its efficacy, either as an adjunctive metric that refines FRAX probabilities and BMD T-scores, or as an independent measure with established clinical cut-off values8.
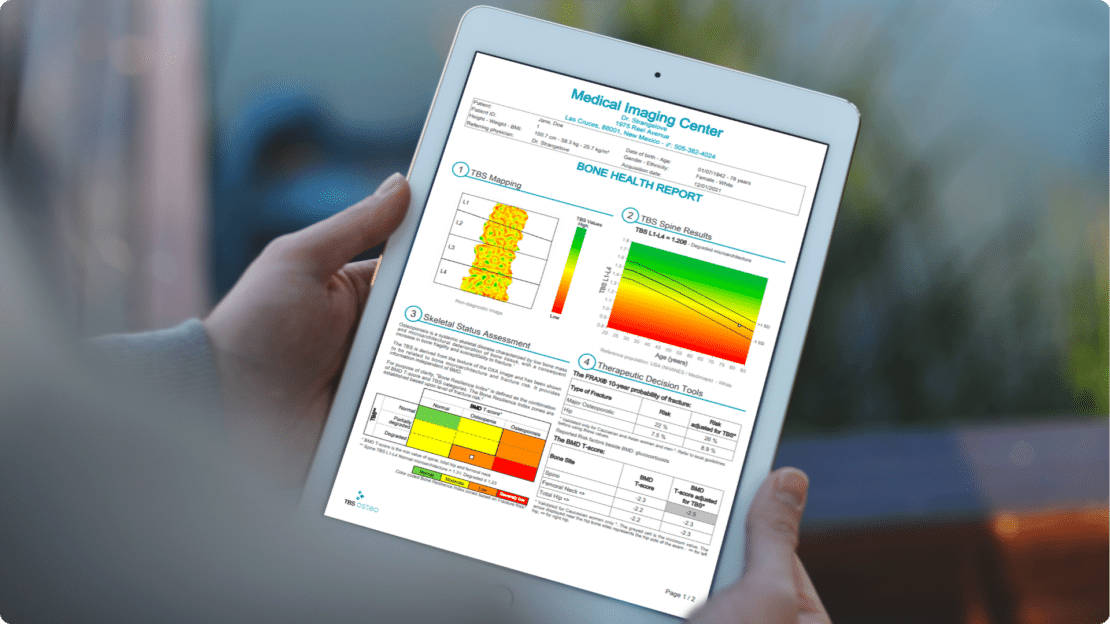

TBS Osteo is an AI-ready technology and state-of-the-art software powered by TBS iNsight to evaluate bone microarchitecture in patients during a DXA bone densitometry scan. It provides the missing link needed to identify more patients at risk of fracture.
1. Kanis JA, McCloskey EV, Harvey NC, Johansson H, Leslie WD. Intervention thresholds and the diagnosis of osteoporosis. J Bone Miner Res. 2015;30(10):1747-53.
2. Siris ES, Chen YT, Abbott TA, Barrett-Connor E, Miller PD, Wehren LE, et al. Bone mineral density thresholds for pharmacological intervention to prevent fractures. Arch Intern Med. 2004;164(10):1108-12.
3. Johnell O, Kanis JA. An estimate of the worldwide prevalence and disability associated with osteoporotic fractures. Osteoporos Int. 2006;17:1726-33.
4. Moran CG, Wenn RT, Sikand M, Taylor AM. Early mortality after hip fracture: is delay before surgery important?. JBJS. 2005;87(3):483-9.
5. Compston J. Reducing the treatment gap in osteoporosis. Lancet Diabetes Endocrinol. 2020;8(1):7-9
6. Pasco JA, Seeman E, Henry MJ, Merriman EN, Nicholson GC, Kotowicz MA. The population burden of fractures originates in women with osteopenia, not osteoporosis. Osteoporos Int. 2006;17:1404-9.
7. Pothuaud L, Carceller P, Hans D. Correlations between grey-level variations in 2D projection images (TBS) and 3D microarchitecture: applications in the study of human trabecular bone microarchitecture. Bone. 2008;42(4):775-87.
8. McCloskey EV, Odén A, Harvey NC, Leslie WD, Hans D, Johansson H, et al. A meta‐analysis of trabecular bone score in fracture risk prediction and its relationship to FRAX. J Bone Miner Res. 2016;31(5):940-8.