Clinical news 26/10/2023
Authors: G. Gatineau1, E H. Ahmed2, K. Hind2, O. Lamy1, E. Gonzalez Rodriguez1, L. Beaugé2,D. Hans1, 2
1Center of Bone Diseases, Rheumatology Unit, Bone and Joint Department, Lausanne University Hospital, & University of Lausanne, Lausanne, Switzerland
2Medimaps group SA, Plan-les-Ouates, Switzerland;
Introduction
Dual-energy X-ray absorptiometry (DXA) is a widely used imaging technique to diagnose osteoporosis based on bone mineral density (BMD). However, the accuracy of DXA for measuring lumbar spine BMD can be limited due to factors such as degenerative changes, osteophytes, and artifacts. These limitations can lead to artificially elevated BMD values, which can result in misdiagnosis and undertreatment of osteoporosis. To address these issues, a new AI-based spine segmentation (SpS) application has been developed (Medimaps Group, Switzerland) to improve the accuracy and efficiency of DXA-based spine BMD analysis. The purpose of this study was to evaluate the effectiveness of this new AI SpS application in improving DXA lumbar spine (LS) BMD
outcomes.
Methods
The study sample comprised 1,052 postmenopausal women (mean age=70.3±7.4 y, BMI=26.0±4.4 kg/m²) from the OsteoLaus cohort who underwent a LS (L1-L4) DXA scan at the third visit (GE Lunar iDXA). Vertebral anomalies, as per the ISCD criteria of a +1 SD T-score difference between adjacent vertebrae, were identified in 568 women. In this sub-sample, LS BMD and T-score were analysed using three different approaches to SpS, including the default DXA manufacturer, the AI application, and the criterion (clinical expert). Statistical analysis was performed using Student’s t-tests to determine differences between outcomes. The impact of each of the three SpS methods on BMD classification was then examined [osteoporosis (LS BMD T-score ≤ -2.5), osteopenic (≤ -1.0), or normal (> -1)]. Contingency tables compared and analyzed sensitivity and specificity for Default and AI classifications. Classification levels of agreement of both default and AI SpS with the Expert were calculated using Kappa index.
Results
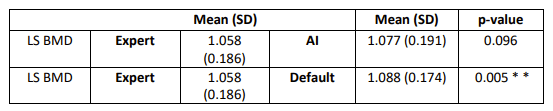
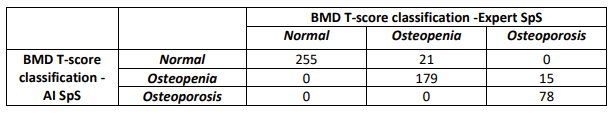
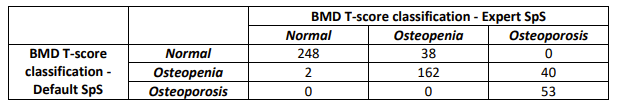
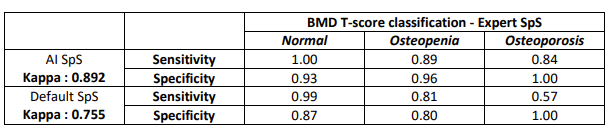
There were significant differences in LS BMD outcomes derived from the Expert and the Default SpS (p=0.005**, Table 1). There were no significant differences in LS BMD derived using the Expert and the AI SpS (p=0.098, Table 1). The prevalence of LS osteoporosis was 16.4% on Expert SpS, 9.3% on the Default, and 13.7% on the AI (Tables 1, 2). Osteoporosis classification sensitivity was 0.57 for the Default SpS, and 0.84 for the AI (Table 3). Kappa indices showed greater agreement between AI and Expert (Kappa=0.892) than Default and Expert classifications (Kappa=0.755).
Conclusion
The AI SpS demonstrated improved LS BMD measurements and greater agreement of densitometric osteoporosis classifications with the expert SpS compared with the default. These results suggest that AI SpS may be a valuable tool to improve the accuracy of LS BMD analysis and individual level diagnosis.